Types of Lymphocytic Alopecia
Alopecia Mucinosa

Alopecia mucinosa, also known as follicular mucinosis, is a condition resulting from the deposition of a jelly-like substance (called mucin) in and around the hair follicles. It can occur as a benign primary condition, of unknown cause, or secondary to other conditions such as atopic dermatitis (eczema) or cutaneous T-cell lymphoma.
The primary form was first described in 1957 by the dermatologist Pinkus, favoring children and adults in their third and fourth decades of life. It may occur as pink plaques on the face or scalp, with associated scale and hair loss. The secondary form represent a slow malignancy, and generally occurs in an older age group with larger areas of involvement on the extremities, trunk and face.
Central Centrifugal Cicatricial Alopecia
Central centrifugal cicatricial alopecia (CCCA) belongs to a group of disorders called cicatricial or scarring alopecias that destroy the hair follicle, replace it with scar tissue, and cause permanent hair loss. The cause is unknown but is probably an inflammatory process induced by genetic or environmental factors.
Women with CCCA develop an area of thinning at the center of their scalp, and this gradually enlarges and spreads outward, hence the name “central centrifugal.” The inflammation that destroys the hair follicle is below the skin surface and there is usually no “scar” seen on the scalp.
The cause of CCCA is unknown. Genetic factors may be important, and inflammation plays a role in the process. The inflammation, in the form of white blood cells, surrounds the hair follicles and gradually destroys them.
 |
 |
 |
CCCA affects primarily women of African descent, but rarely occurs in women of other ethnic groups and men. It usually presents in individuals 25-65 years of age. There have been several reports of CCCA occurring in families and genetic studies are currently underway to further identify possible contributing genes. However, most patients with CCCA have no family history of a similar condition. CCCA is not associated with any other illnesses.
In many cases, the area of hair loss of CCCA is not accompanied by any symptoms. In some cases, the hair loss is associated with itching, burning, tenderness, pain, or a tingling sensation. The bare area gradually enlarges and may affect a large portion of the central scalp with only few solitary hairs remaining.
Two other hair problems, hair breakage and traction alopecia (hair loss along the hairline), may be present in some women with CCCA, but it is not clear if they are at all related to the scarring process. Hair breakage and traction alopecia are both due to hair styling and hair grooming practices and the relationship to the development of CCCA is still being determined.
Chronic Cutaneous Lupus Erythematus / Discoid Lupus

Discoid lupus erythematosus (DLE) is cutaneous manifestation of the autoimmune spectrum of lupus erythematosus. It is further classified as a form of chronic cutaneous lupus erythematosus which primarily affects the skin and hair follicles.
DLE is not considered a primary cicatricial alopecia, because the inflammation surrounds not only the hair follicle but many other structures in the skin. If treated early, hair loss in DLE is potentially reversible. If not treated early, over half of affected patients will develop scarring alopecia.
Cause
Like many autoimmune disorders, the true cause is unknown. It likely is caused by a combination of genetic susceptibility, environmental triggers, and other factors including medications and other medical comorbidities.
Signs & Symptoms
DLE is more common in women, especially women of African ancestry. It may occur at any age, but onset is frequently in persons between age 20 and 40 years. Few patients (5 to 10%) with DLE progress to SLE, although in patients with classic SLE, DLE occurs in about 20% of patients.
DLE most commonly affects the scalp, face, and ears. It starts as a well-defined scaly purplish patch and enlarges into a discoid (coin-shaped) patch of hair loss. Decreased or increased pigmentation, increased blood vessels, and follicular plugging are characteristically seen in the center of the of discoid lupus lesions.
Another helpful finding is the “carpet tack” sign that may be elicited by lifting the adherent scale and revealing spikey keratin on the underside. External ear involvement is common in patients with discoid lupus. Symptoms may include itching, pain, burning, and tenderness.
Classic Pseudopelade (Brocq)

Pseudopelade is a type of scarring hair loss condition. The hair loss in the bald areas is permanent. Both men and women can develop pseudopelade, although it is 3 times more common in women.
Several features lead to this diagnosis, including areas of scarring hair loss, some redness around the hair follicles, depression of the skin, and findings on the biopsy showed very little inflammation, loss of the fat glands and scarring
Pseudopelade is challenging to treat. Even with treatment, some cases to spread, albeit very slowly.
Pills may be used such as doxycycline, Plaquenil, isotretinoin (Accutane), and mycophenolate mofetil. Injection of steroids may be advised. Use of topical medicines you apply yourself at home may also be advised (Clobetasol, Protopic, Clobex).
We encourage you to discuss these treatment options with your dermatologist.
Pseudopelade, French for “imitator of alopecia” describes a type of scarring hair loss that at first glance looks like alopecia areata (a non-scarring form of hair loss). But on closer inspection one sees smooth shiny patches of hair loss with loss of follicular openings.
The term has been confusing because it can represent either new onset scarring alopecia with no evident inflammation or symptoms, or late-stage lichen planopilaris which is considered ‘burnt-out.” Many have suggested that the term be abandoned in favor of a late stage LPP.
Frontal Fibrosing Alopecia
Frontal fibrosing alopecia (FFA) is a form of hair loss that can be permanent or scarring in nature. It is currently classified as a subtype of lichen planopilaris. The cause is unknown but is probably an inflammatory process induced by genetic or environmental factors.
It is classified as a primary inflammatory scarring type of hair loss. That is, it is not from infections, burns, surgical scars, caustic hair products, etc., but is a disease centered around the hair follicle unit itself. Women with FFA develop mild to extensive hairline recession that can expand around the perimeter of the scalp. Total eyebrow loss can occur as well.
Cause
The cause of frontal fibrosing alopecia is unknown. Over the past few decades there has been an exponential increase in the number of new cases, especially in westernized countries. This has lead researchers to believe that there may be an underlying environmental trigger.
Recent epidemiologic studies have suggested that leave-on cosmetic products (sunscreen, makeup, etc.) may be linked to the cause, since their use has dramatically increased in the past few decades. However, more research is needed on this topic.
Because this disease affects peri- and post-menopausal women predominantly, it has been hypothesized that a relative lack of estrogen or hormonal shifting may trigger the onset of the disease.
Like its parent diagnosis, lichen planopilaris, the target of inflammation is the sebaceous or oil gland which is located at the same site as the stem cell region of the hair follicle. Recent research has shown that there is a defect in a “master regulator” protein called the peroxisome proliferator-activated receptor gamma, or PPAR gamma.
PPAR gamma is responsible for the preservation of hair follicle cells, including stem cells and sebaceous glands. Loss of PPAR gamma leads to sebaceous gland dysfunction, which causes abnormal processing and buildup of “toxic” lipids.
This abnormal buildup of lipids triggers inflammation that destroys the oil gland inflammation and the nearby stem cells, which are innocent bystanders. Once stem cells are destroyed, the follicles cannot regenerate and permanent hair loss ensues.
Signs and Symptoms
The typical profile of a person with frontal fibrosing alopecia is a peri- or post-menopausal adult female. There are isolated cases of it affecting adult males and teenage girls.
 |
 |
 |
Unlike lichen planopilaris, frontal fibrosing alopecia is largely without symptoms. Because the disease is silent it often goes unnoticed for many years before it is diagnosed. There is a triad of findings in fibrosing alopecia which includes:
(1) Sudden eyebrow loss. This can diffuse or patchy loss, and most of the time is accompanied by redness and scaling around the hair follicles. The existing eyebrow hairs themselves may change texture and become course and wiry. Over time, complete permanent eyebrow loss can occur.
(2) Hairline recession. As the name of the disease implicates, the frontal hairline is most often affected, followed by the sideburns, around the ears, and the posterior hairline. The hair loss is band-like and can recess further from the natural hairline if the disease is untreated. The hair follicles surrounding the hair loss have characteristic redness and scaling around the hair follicles.
(3) Extremity hair loss. This is a more inconspicuous finding, because extremity hair loss can also happen naturally as we age. However, hair loss on your extremities, like arms and legs, in frontal fibrosing alopecia can be patchy and completely devoid of hair, which is an unusual pattern for age-related hair loss.
Other findings of frontal fibrosing alopecia include skin-colored facial bumps, or papules, which represent involvement of the vellus (fine, non-pigmented hairs) of the facial region. Sometimes frontal fibrosing alopecia can overlap with classic lichen planopilaris.
Graham-Little Syndrome
Symptoms and Causes
This is a rare condition that presents with a combination of lichen planopilaris of the scalp, lichen planopilaris of the body, and non-scarring hair loss in the axillary or pubic regions. These can present simulataneously or over a period of several months.


Keratosis Follicularis Spinulosa Decalvans
This condition typically begins in childhood. Skin-colored bumps around hair follicles (follicular spines) can be seen in the scalp but also in the eyebrows, eyelashes, and the on the back of the hands and fingers. Sometimes thickening of the skin of the palms and heels may occur. By puberty, many of the follicular spines have disappeared and are replaced by thinning or atrophy of the skin and can eventually lead to scarring alopecia.
The hair loss is often patchy and is rarely total. Eye irritation due to distorted eyelashes and other eye disorders have been reported to occur with this condition.
Cause
KFSD is an inherited disorder with family studies suggesting an X-linked dominant inheritance pattern, though other inheritance patterns have been reported. Men are often more severely affected than women.
Lichen Planopilaris
Lichen planopilaris (LPP) is a form of hair loss that can be permanent or scarring in nature. The cause is unknown but is probably an inflammatory process induced by genetic or environmental factors. It is classified as a primary inflammatory scarring type of hair loss. That is, it is not from infections, burns, surgical scars, caustic hair products, etc., but is a disease centered around the follicular unit itself.
Cause
The cause is unknown but is probably an inflammatory process induced by genetic or environmental factors. The primary target of inflammation in lichen planopilaris is the sebaceous or oil gland which is located at the same site as the stem cell region of the hair follicle.
Recent research has shown that there is a defect in a “master regulator” protein called the peroxisome proliferator-activated receptor gamma, or PPAR gamma. PPAR gamma is responsible for the preservation of hair follicle cells, including stem cells and sebaceous glands. Loss of PPAR gamma leads to sebaceous gland dysfunction, which causes abnormal processing and buildup of “toxic” lipids.
This abnormal buildup of lipids triggers inflammation that destroys the oil gland inflammation and the nearby stem cells, which are innocent bystanders. Once stem cells are destroyed, the follicles cannot regenerate and permanent hair loss ensues.
It is not currently known if lichen planopilaris is truly an autoimmune disorder. Most leaders in the hair loss field feel as though it is not autoimmune, for several reasons: (1) It does not follow familial inheritance patterns of other autoimmune disorders. In other words, the disease arises quite sporadically and not in association with other known autoimmune disease. (2) The dramatic rise of lichen planopilaris in the last 10-20 years does not follow the incidence and prevalence trends for other autoimmune disorders. (3) No autoantibodies have been discovered yet for lichen planopilaris.
Symptoms
Lichen planopilaris affects primarily middle-aged women, but it can also affect men and individuals as young as teenagers.
Lichen planopilaris can be very symptomatic with intense burning, itching, or tingling or it may be largely asymptomatic. Sometimes heavy shedding can be accompanied during periods of high disease activity.
The course of lichen planopilaris is variable. It may evolve slowly with a few patches of hair loss or diffuse central hair thinning, which slowly progresses over many years. In other cases, the course is rapid, and within a few months many patches of hair loss or diffuse thinning spreads over large areas of the scalp. Although uncommon, some patients will have periods of time when the disease is not active (remissions).
On clinical examination, the hair loss is either patchy or diffuse (or both). Typically, the top or crown of the scalp is initially affected, but lesions can occur anywhere on the scalp. Small bare patches may slowly coalesce with others and enlarge to involve large areas.
In a typical active bare area, the center is smooth and devoid of follicular markings. Hair follicles around the margins of the bare areas show perifollicular erythema and perifollicular scale.
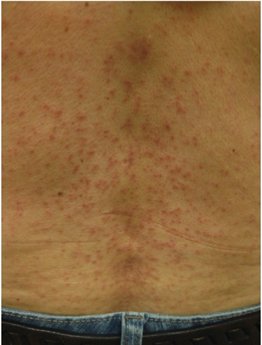
It has been recently recognized that hypothyroidism has been associated with LPP. Some patients with lichen planopilaris of the scalp may also have other forms of lichen planus, most often oral and/or genital lichen planus. Occasionally patients will have cutaneous lichen planus, which presents as very itchy purplish polygonal raised lesions on the trunk or extremities. Let your dermatologist know if you are suffering from other rashes, mouth sores, or genital sores, in addition to your hair loss.
Hair Loss Treatments in Kansas City & Liberty, MO
At Darling Hair Restoration, hair transplant surgeon Dr. Scott Darling provides treatment for hair loss caused by lymphocytic alopecia. Contact our hair transplantation clinic in Liberty, Missouri, today at (816) 792-3400 or request an appointment using our online form.

